New Medicare Numbers to Have Limited Impact on MSP Compliance Processes
July 12, 2018
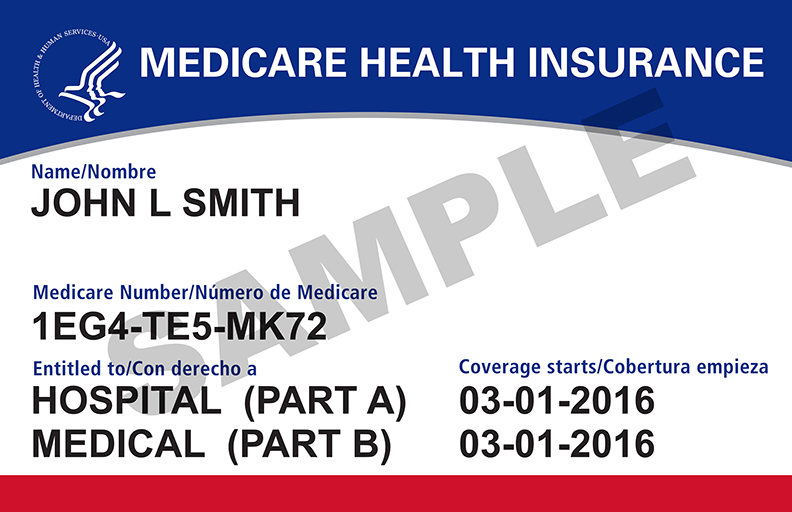
Since April 2018 the Centers for Medicare and Medicaid Services (CMS) has been issuing new Medicare identification numbers to some 60 million active Medicare beneficiaries. Pursuant to the Medicare Access and CHIP Reauthorization Act (MACRA) of 2015, a Medicare Beneficiary Identifier (MBI) is replacing the Social Security Number (SSN) based Health Insurance Claim Number (HICN) on all Medicare cards issued to beneficiaries. An MBI is a unique, randomly generated alphanumeric identifier which will no longer include any portion of a person’s SSN. The primary reason the identifiers are being replaced is to limit identity theft associated with use of SSNs in Medicare IDs.
The process of issuing new Medicare cards with MBIs is to be completed by April 2019. Medicare beneficiaries and medical providers requesting payment by Medicare can continue to use either the HICN or MBI through December 31, 2019. However, as of January 1, 2020, Medicare beneficiaries and medical providers must use the MBI to access Medicare-covered medical care and when requesting payment by Medicare for such care.
Limited Impact on MSP Compliance
While the statute requires CMS remove the SSN from Medicare IDs, it leaves an exemption allowing CMS to continue to utilize SSNs for purpose of Medicare Secondary Payer data exchanges and processes. Accordingly, for purposes of Section 111 Mandatory Insurer Reporting, Responsible Reporting Entities (RREs), may continue to use SSNs, HICNs or MBIs post January 1, 2020. However, when querying a claimant for Medicare beneficiary status or otherwise updating a report, if an MBI has been issued to the beneficiary, then the response file from CMS will be the MBI, not the HICN.
In regard to communication with the Benefits Coordination and Recovery Center (BCRC) and Commercial Repayment Center (CRC), SSNs, HICNs or MBIs may be utilized to ID the beneficiary. Correspondence from these entities, such as Conditional Payment Letters and Demands, will include either an HICN or MBI, depending upon the beneficiary ID which was most recently reported.
As for communication with the Workers Compensation Review Contractor pertaining to MSA submissions, SSNs, HICNs or MBIs may be utilized. Correspondence from the WCRC/CMS will include whatever beneficiary ID was submitted with the MSA proposal.
From a practical standpoint, what employers, carriers and other payers need to be aware of is they will increasingly be seeing these MBIs from claimants and responses from CMS and CMS contractors.
Tower MSA Partners will continue to monitor the transition from HICNs to MBIs and its impact on the MSP process. Any relevant updates will be provided with a breakdown of the implications to your practices and processes. If you have any questions please contact Dan Anders, Chief Compliance Officer, at 888.331.4941 or Daniel.anders@towermsa.com.

