As we come to the end of 2019, put on your party hats, toot your horns and clink your champagne glasses, as we introduce Tower’s MSP Compliance Countdown. The MSP Compliance Countdown provides a quick summary of, in our opinion, the top ten Medicare Secondary Payer compliance stories in 2019. So, start dropping the MSP compliance ball and here we go:
10. Electronic
Payment Option Added to MSPRP – On April 1, 2019, the Centers for
Medicare and Medicaid Services (CMS) added an option to the Medicare Secondary
Payer Recovery Portal (MSPRP) allowing for reimbursement of Medicare
conditional payment demands by direct payment from a checking or savings
account, debit card or PayPal. While
convenient for Medicare beneficiaries, insurer and employer payers say this
does not work with their payment processes. It is our understanding that CMS
may consider expanding this option to other payment methods in 2020.
9. U.S.
Attorney Again Takes on Plaintiffs’ Attorneys for Failure to Reimburse Medicare
– On March 18, 2019, the U.S. Attorney for the District of Maryland announced a
$250,000 settlement agreement with the law firm of Meyers, Rodbell &
Rosenbaum, P.A., as a result of allegations the firm failed to reimburse the
United States for Medicare payments made to medical providers on behalf of a
firm client. This followed a 2018 action
by a U.S. Attorney in Pennsylvania who reached a $28,000 settlement with a
plaintiffs’ firm for failing to reimbursement Medicare. Notably, just last month, the Maryland U.S.
Attorney obtained a $90,000
settlement from a plaintiffs’ firm that had referred the case to
co-counsel.
8. Open Debt
Reports Available in the MSPRP – A 2019 update to the MSPRP provides a
useful tool for insurer and self-insured entities to identify outstanding or
unknown Medicare conditional payment demands.
Called the Open Debt Report, it is available to insurers and
self-insured organizations, or as CMS calls them Responsible Reporting Entities
(RREs), that have registered for MSPRP access (Tower can also access the
reports when it is the Recovery Agent for the RRE).
7. Self-Reporting
Functionality Added to MSPRP – In January, CMS added a self-reporting
function to the MSPRP enabling MSP cases to be reported through the portal
versus via phone or written correspondence to the Benefits Coordination &
Recovery Center (BCRC). Primarily a
time-saving measure, it is a welcome improvement over having to speak to a BCRC
representative who takes down the claim information and enters it into their
system.
6. Update
to CMS WCMSA Reference Guide Clarifies Lyrica Policy – Throughout 2018, CMS
increasingly added Lyrica (brand-name only at the time) to MSAs for diagnoses that
had previously been considered non-Medicare covered. In a January update to its reference guide,
CMS clarified its reasoning for considering Lyrica Medicare-covered for radicular
pain stemming from the spinal cord (cervical, thoracic and lumbar), even when
there is no evidence of what is defined as a “traumatic” spinal cord injury.
5. CMS
Adds Electronic Submission Option for MSA Attestations – On October 7,
2019, CMS released an updated Workers’ Compensation Medicare Set-Aside Portal
(WCMSAP) User Guide which added the capability for both self- and professional-MSA
administrators to electronically submit annual attestations for CMS-approved
MSAs. Previously, the sole option for an MSA administrator was to
complete the attestation form and submit to Medicare’s BCRC via mail. Electronic
submission of annual attestations benefits both CMS and MSA administrators as it
facilitates better and faster coordination of benefits.
4. Proposed
Rules on LMSAs and Section 111 Penalties Again Delayed – The wait continues
for CMS to issue proposed rules on Liability MSAs (LMSAs) and Section 111 Mandatory
Insurer Reporting penalties. CMS’s first
notice in December 2018 indicated the proposed rules would be issued in
September 2019. Subsequent notices moved
the date to October 2019 and we now have notices moving the date for issuing
the proposed rule on penalties to December 2019 (no rule have been released as
of the date this article was published) and for rules on LMSAs to February
2020.
3. Lyrica
Goes Generic – In July 2019, the FDA approved multiple applications for
generic Lyrica. While not directly
related to MSP compliance, this action has a notable impact on MSA allocation
amount given the above-noted use of Lyrica for neuropathic back pain. Lyrica went from $9.36 for a 50 mg pill at
brand name to $0.90 today for the generic, effectively removing it as a
significant cost-driver in the MSA.
2. CMS
Expands MSA Amended Reviews & Modifies Consents to Release in Updated
Reference Guide – In October 2019, CMS released an updated WCMSA Reference
Guide which expanded the Amended Review MSA lookback from four to six years
post the prior MSA approval. It also
introduced some additional language to the Consent to Release form which
requires the claimant to initial that the WCMSA was explained to him or her and
that he or she approves of the contents of the MSA submission. While the expansion of the Amended Review MSA
is welcome news, the revised Consent to Release form, which becomes effective
4/1/2020, may cause delay in the MSA submission process.
1. U.S.
Appellate Court Holds Guaranty Fund Not a Primary Plan under the MSP Act – In
an October 10, 2019 decision from the U.S. Court of Appeals for the Ninth
Circuit, the California Insurance Guarantee Association (CIGA) was found not to
be a primary plan under the Medicare Secondary Payer (MSP) Act. The result of this decision, if not reversed
on appeal, is that CIGA would have no responsibility to reimburse Medicare for
conditional payments or to allocate funds in a Medicare Set-Aside (MSA) for
future medical.
We chose the CIGA decision as #1 in our countdown because it
stands for the principle that we should not readily accept everything CMS says
as gospel. While CMS rightly works to
protect the Medicare trust fund, it should be challenged when it goes beyond
its statutory and regulatory authority or does not even follow its own MSA
review policy.
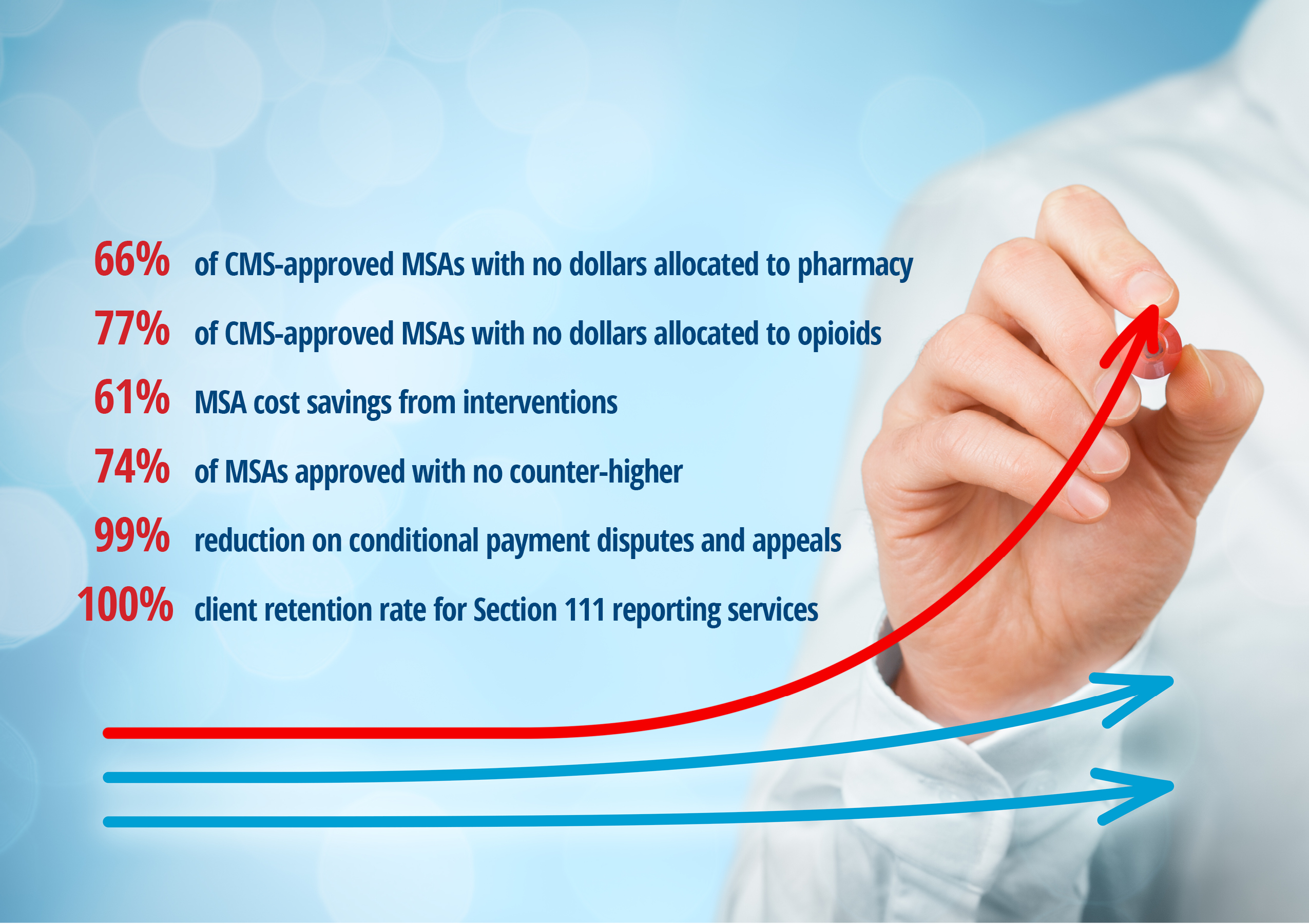
Every day Tower challenges CMS, whether it is the result of
overinclusive Medicare conditional payments or unnecessary or mispriced medical
care allocated in an MSA. Notably, this
year Tower repeatedly challenged CMS’s inclusion of urine drug screens in MSAs
where there was no past history of use.
The result, CMS corrected its policy, saving employers and carriers tens
of thousands of dollars.
If we can leave you with one New Year’s resolution, it is to
not be afraid of challenging CMS, when warranted. Tower will certainly continue to so on your
behalf in 2020.
May you have a warm and wonderful holiday and all the best
in the new year.